Autism research has come a long way in identifying genetic and environmental contributors, but recent findings are shedding new light on a less explored factor: the mother’s gut microbiome. A study published in The Journal of Immunology suggests that microbial activity in the maternal gut may influence fetal brain development through immune system signaling, offering a new perspective on how autism-related traits may begin to form before birth. While the study was conducted in mice, the mechanisms it uncovers—particularly the role of an immune molecule called IL-17a—could help explain how prenatal biological conditions contribute to neurodevelopmental disorders.
This research doesn’t claim to offer definitive answers or immediate clinical applications, but it opens up an important area of investigation. It also reinforces a broader point that’s becoming harder to ignore: maternal health—especially gut and immune health—has far-reaching effects on the developing child. As science begins to connect the dots between microbiota, inflammation, and early brain development, the case for including gut health in prenatal care becomes stronger and more urgent.

The Gut-Brain Connection Starts Before Birth
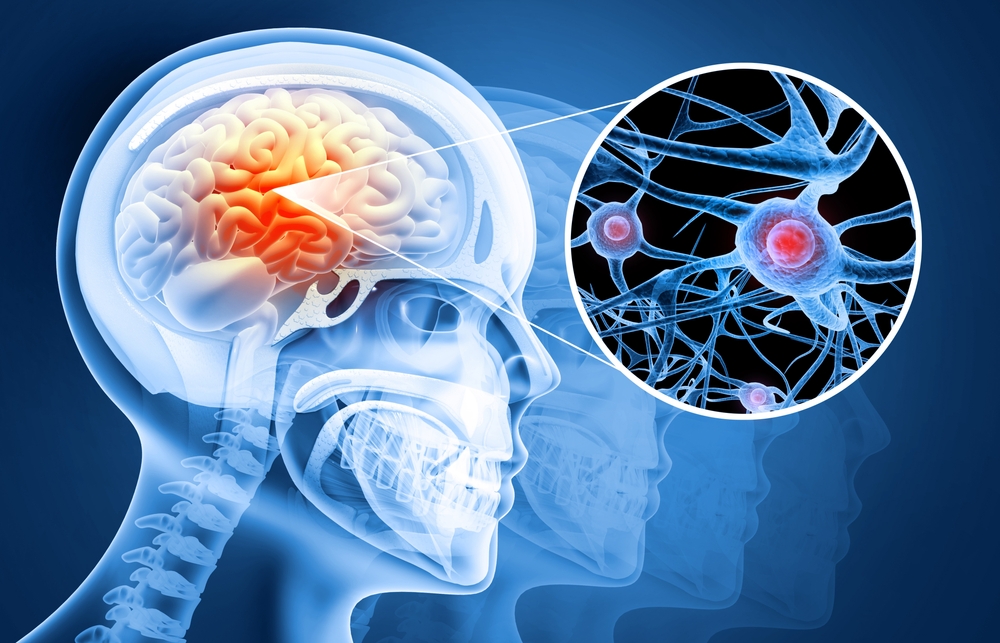
The connection between gut health and brain development isn’t new, but recent research has started to zero in on how this relationship could play a role in autism. A study published in The Journal of Immunology provides evidence that a mother’s gut microbiota may shape the development of her child’s brain long before birth. Specifically, researchers found that certain microbial compositions in the mother’s gut could influence the likelihood of autism-like behaviors in offspring—at least in mice.
Here’s the key finding: when pregnant mice had gut microbiota that triggered higher levels of an immune molecule called IL-17a, their offspring were more likely to develop autism-like traits, such as altered social interactions and repetitive behaviors. IL-17a isn’t just a random immune marker—it’s been linked to inflammatory diseases like multiple sclerosis and psoriasis, and plays a role in protecting the body from infections. But in this context, it appears to also affect the brain’s development in utero.
When researchers suppressed IL-17a during pregnancy, the offspring didn’t develop these behaviors, suggesting a strong link between maternal immune activity and neurodevelopmental outcomes. To further validate the role of gut microbes, they transplanted fecal material from mice with the autism-linked microbiota into healthy mice. The result? The second group’s offspring started showing the same autism-like traits. This confirmed that the maternal microbiota—not just genetic or environmental factors—can influence brain development in significant ways.
While these findings are based on animal models, they open up important questions for human health: What microbes in the maternal gut influence IL-17a production? Could adjusting gut health before or during pregnancy lower autism risk in children? These are now pressing topics in autism research, and they emphasize the growing importance of maternal microbiome health—not just for digestion, but for the developing brain.

The Role of IL-17a – More Than Just an Immune Molecule
IL-17a is a cytokine, a type of protein the immune system uses to coordinate defense against infections. It has been widely studied for its role in autoimmune conditions like multiple sclerosis and psoriasis, but this molecule is now drawing attention for its potential influence on fetal brain development. In the recent mouse study, elevated levels of IL-17a in pregnant females—driven by specific gut microbes—correlated with offspring developing autism-like behaviors, including reduced social interaction and increased repetitive behaviors. The link was strong enough that when researchers suppressed IL-17a during pregnancy, the offspring did not show these behavioral differences, even when the mother’s gut microbiota would have otherwise triggered them.
This finding suggests IL-17a may act as a bridge between the maternal immune response and fetal neurodevelopment. Importantly, IL-17a isn’t inherently harmful; it plays a protective role in guarding against infections, particularly fungal ones. But when its levels rise in response to inflammation during pregnancy, it may influence how the brain forms and functions in ways that carry long-term effects. The research doesn’t suggest IL-17a alone causes autism, but rather that it might be one piece of a complex puzzle—especially when combined with certain microbial patterns in the mother’s gut.
Researchers were able to replicate the autism-like traits by transferring fecal microbes from high-IL-17a-producing mothers into previously unaffected ones, strongly implicating the microbiota as the source of the immune activation. This underscores a key point: it’s not just the presence of IL-17a, but how the maternal immune system is primed by gut bacteria that matters. The findings suggest that maternal inflammation, shaped by the microbiome, can impact fetal brain development in measurable ways. That insight could eventually shift how we think about prenatal care, particularly around maternal gut health, inflammation, and immune regulation.
Although the study was done in mice and may not directly translate to humans, it introduces a promising area of exploration. Understanding what drives excessive IL-17a responses during pregnancy—and whether certain microbial profiles make this more likely—could lead to new preventive strategies. The goal isn’t to eliminate this immune response entirely, but to maintain a healthy balance that supports both maternal immune protection and optimal fetal development.

Why Maternal Microbiota Matters More Than the Infant’s
One of the more surprising outcomes of the study was that the mother’s microbiota—not the infant’s own—was the key factor influencing autism-like behavior in the offspring. This challenges a common assumption that the child’s gut health is the primary driver of early neurodevelopment. According to the research, what happens during gestation—specifically how the maternal microbiome interacts with the immune system—sets the stage for how the fetal brain develops.
To test this, researchers worked with two groups of mice from different labs. One group had gut bacteria that primed their immune system for inflammation via IL-17a, while the other group did not. When IL-17a was suppressed in both groups, their offspring showed normal behavior. But when left untreated, only the offspring of the first group—those with the inflammation-prone microbiota—developed autism-like traits. This indicated that the mother’s immune environment, shaped by her gut microbes, had a lasting impact on brain development in the fetus.
To go further, the researchers transplanted gut bacteria from the inflammation-prone group into the microbiota-stable group. Once the healthy mice acquired the altered microbial community, their offspring also began showing the same autism-like behaviors. This confirmed that the maternal microbiome, not genetic differences between the mice, was responsible. It’s a significant insight: even without changing the genetic code, altering gut bacteria in the mother alone was enough to influence behavioral outcomes in the next generation.
This reinforces the idea that maternal gut health plays a central role in shaping not just immediate outcomes like birth weight or immunity, but also long-term neurodevelopmental health. While human studies are still needed to confirm these effects, the data suggest that prenatal interventions focused on gut health—dietary changes, probiotics, or other microbiome-targeted strategies—could eventually become part of broader maternal health recommendations.

Practical Ways to Support Gut Health During Pregnancy
For expecting mothers, maintaining a balanced gut microbiome might be more important than previously understood—especially in light of research linking maternal microbiota to fetal brain development. While the science is still evolving, there are several evidence-backed steps that can help support gut health during pregnancy without overcomplicating things or promoting unproven interventions.
First, a diverse, fiber-rich diet is one of the most effective ways to nourish beneficial gut bacteria. Foods like vegetables, fruits, legumes, and whole grains feed microbes that produce short-chain fatty acids, which support a healthy gut lining and reduce inflammation. Avoiding overly processed foods and added sugars also helps prevent imbalances in gut flora that may lead to low-grade inflammation—something particularly important during pregnancy when immune activity is already heightened.
Second, fermented foods such as yogurt with live cultures, kefir, sauerkraut, and kimchi can introduce or reinforce populations of helpful bacteria. These foods aren’t a cure-all, but they do contribute to microbial diversity, which is a hallmark of gut health. For women who can’t tolerate fermented foods or have specific dietary needs, certain probiotics may offer benefits. However, not all probiotics are equal—products should contain well-studied strains and be third-party tested for quality. It’s always best to discuss probiotic use with a healthcare provider, especially during pregnancy.
Third, managing stress is often overlooked but critical. Chronic stress can alter gut microbial composition and increase inflammation. While pregnancy comes with its own physical and emotional pressures, practices like regular movement, sleep hygiene, and mindfulness-based techniques (like short breathing exercises) can support both mental and gut health.
Finally, it’s worth being cautious with unnecessary antibiotics. These medications can dramatically reduce gut microbial diversity, sometimes with long-lasting effects. Of course, antibiotics should be used when medically needed, but their use should always be guided by a clear clinical indication, especially during pregnancy.

Moving Toward Prevention—What This Means for Future Research and Public Health
The findings from this study don’t offer a cure or diagnostic test for autism, but they do represent a shift in how researchers think about its early biological underpinnings. For years, autism research has largely focused on genetics and postnatal environmental factors. This new evidence adds another dimension: maternal gut health and immune signaling during pregnancy could play a meaningful role in shaping the neurological development of the fetus. While these findings are based on animal models and can’t yet be applied directly to human pregnancies, they help clarify the biological pathways that could one day be targeted for prevention or risk reduction.
What stands out in this study is how a change in the mother’s microbiota—without any genetic manipulation—was enough to alter neurodevelopmental outcomes in offspring. This suggests that interventions during pregnancy may eventually become part of strategies to support optimal brain development in children, similar to how folic acid supplementation is now standard for preventing neural tube defects. Researchers are already working to identify which specific microbes or microbial metabolites influence immune molecules like IL-17a, and whether patterns found in mice can be confirmed in human studies. This kind of research takes time, but it opens up real possibilities for developing targeted nutritional or microbiome-based interventions during pregnancy.
At the public health level, this line of research could eventually lead to broader recommendations for prenatal care that go beyond standard nutrition and screenings. For example, future guidelines might include personalized assessments of gut health or microbial diversity as part of routine maternal health checks. There could also be new educational efforts aimed at helping women understand the importance of gut health not just for digestion, but for long-term outcomes in their children. That said, it’s important to avoid overstating what we know so far. The role of IL-17a and the maternal microbiome is one piece of a larger, complex picture involving genetic, environmental, and epigenetic factors.
The key takeaway for now is this: maternal health is deeply interconnected with early childhood development in ways we’re just beginning to understand. Supporting gut health during pregnancy is a low-risk, potentially high-reward approach, but it’s not a guaranteed solution or a standalone fix. Still, research like this adds urgency to the broader conversation about how we support women’s health during pregnancy—not just in terms of avoiding harm, but actively promoting conditions that give the next generation the best possible start.













Leave a Reply