 BBC
BBCThe number of 16-24 year olds in England reporting symptoms of obsessive compulsive disorder, or OCD, has more than tripled in a decade, BBC analysis of NHS data has found.
The condition is now the second-most widespread mental health disorder for young adults, according to statistics from a major NHS England survey.
“OCD, I like to think of it as a bully, it attacks everything, everything you care about, everything you love,” says Sophie Ashcroft.
“A lot of people do associate OCD with cleanliness, and being clean, and getting all your socks in a certain order. It’s so much more than that.”
The 22-year-old is one of a number of young people and their families to have contacted us through Your Voice, Your BBC News explaining how they can’t access NHS treatment for their symptoms.
Those who could get seen spoke of a shortage of expert staff and effective treatments.
The average referral time figure for young people to be seen at a national OCD centre in London was 41 weeks last year, nearly three times as long as it was five years previously.
The government told us it was “turning services around”, hiring 8,500 extra mental health workers, delivering more talking therapies and providing better access to help through the NHS App. It also said it was expanding the rollout of mental health support teams in schools.
Sophie sometimes struggles to leave her home because she feels compelled to repeat small tasks – such as getting into the shower or cleaning her teeth – to dispel intrusive or distressing thoughts.
“If I had a bad thought during the day, it would ruin the rest of my day. I’d think something bad was gonna happen,” she tells us.
‘Behind closed doors it’s sheer panic’
The people who have contacted BBC News say lives have been devastated, with some families who haven’t been able to get NHS help telling us they have spent hundreds of thousands of pounds on private care.
Charities insist there is an OCD crisis and say the figures should be a wake-up call for the government.
OCD symptoms can affect adults and children, and can begin as early as six years old – but they are often triggered during puberty and early adulthood.
Sophie’s symptoms first appeared when she was aged nine, she says, but it was a decade later, when a close friend died, that things became a lot worse.
To dispel troubling thoughts, she says it led her to repeat actions again and again – things most people would consider mundane and would do without a second thought.
“It’s something telling me you have to do that again, you have to hug that person again, and it just takes over,” says Sophie. “It’s such an awful, awful feeling.”
Despite all this, Sophie has just finished drama school. “I’m really, really good at hiding it, but behind closed doors it’s sheer panic,” she explains.
 Getty Images
Getty ImagesAbout 370,000 young people in England reported OCD symptoms in the financial year 2023/24, our analysis of the latest NHS Adult Psychiatric Morbidity Survey (June 2025) has found.
That is more than three times the number from 2014, when the figure stood at around 113,000.
It means OCD is now second in the list of named mental health disorders – placing it and other anxiety disorders well ahead of depression:
- Generalised anxiety disorder (GAD) 7.6%
- Obsessive compulsive disorder (OCD) 5.7%
- Depressive episodes 3.8 %
Why is OCD on the rise among young people?
Improved awareness of the condition has likely contributed to people seeking help, say experts – but, according to charities and many of those with OCD, societal problems, combined with the pressure of social media, are the main driver for the reported rise.
Leigh Wallbank, chief executive of charity OCD Action, describes many young people’s lives as a “pressure pot”.
“They’re facing financial issues, educational issues, global issues – the environment is such a big issue,” she tells us. “I think of them living in this pressure pot, and then underneath that, giving heat to this pressure pot, is social media.”
The Covid-19 pandemic also played a part, says Minesh Patel, associate director of policy and influencing at the mental health charity, Mind.
The pandemic put a “particular and unique strain” on people with OCD, with disruption to routine, an inversion of social norms and a hyperfocus on hygiene, he says.
“Barriers to social interaction, including treatment and support services, meant that many coping mechanisms were disrupted or unavailable for an extended period of time,” he adds.
NHS help for OCD patients includes specialist talking therapy called Cognitive Behavioural Therapy (CBT) – which can include Exposure and Response Prevention (ERP).
Through ERP patients are helped to manage their anxiety by gradually being exposed to their fears, while preventing them from performing their usual compulsive behaviours.
Medication is also offered – usually a type of antidepressant.
 Getty Images
Getty ImagesBut not everyone can access these treatments.
Sophie was told by her GP that it is likely she does have OCD – but, two years on, she still hasn’t received an appointment to see a specialist for a formal diagnosis.
In the meantime, her GP has referred her for a limited course of CBT which comes to an end soon. Sophie says she is “absolutely petrified” of what the future holds.
Leigh Wallbank from OCD Action is critical of the government for failing to collect regular quarterly data on obsessive compulsive disorder, and outcomes for patients who have it, as it does for many other conditions.
Without data, says the charity, the NHS is blind to the real scale of OCD, the success of treatments and who is being left behind.
We asked health officials in Scotland, Wales and Northern Ireland if they knew the number of young people with OCD symptoms, but they all said they do not collect that information.
‘The system could not, or would not, provide help’
A mum from the south of England, who wants to remain anonymous, told us her autistic daughter first showed signs of OCD when she was 10 years old. Her daughter is now 17 and the OCD is severe, she says.
“My daughter has gone from being a scholarship-winning student, to being sectioned multiple times.”
Some specialist treatment has been offered to the teenager, but her mum tells us her daughter is often too unwell to leave the house to attend appointments, or even take her medication.
“The impact on [all] our children, and us, is devastating. Our lives have been decimated not just by the illness, but by a system that could not, or would not, provide the help she needed, when she needed it.”
The mother says the UK is failing in its treatment of young people with severe OCD. There are not enough specialists, beds or treatment options, she believes.
Children and adolescents with OCD across England can receive treatment at a national centre at the Maudsley Hospital in London.
However, the average wait time for a referral to the service rose from 15 weeks in 2020, to 41 weeks in 2024, according to a response to the BBC’s Freedom of Information Act request.
But the hospital trust says that wait time is being cut.
Ade Odunlade, chief operating officer for South London and Maudsley NHS Foundation Trust said: “We have worked incredibly hard to reduce delays and have lowered the average wait for assessments to around 20 weeks.
“We empathise with anyone who has had to wait for their assessment as we know how difficult that is.”
The trust says it has now been able to secure additional funding which will allow them to employ further staff and drive down the waiting list even further.
It expects an approximate wait for assessment of about 12-16 weeks by early Spring 2026, it told us.
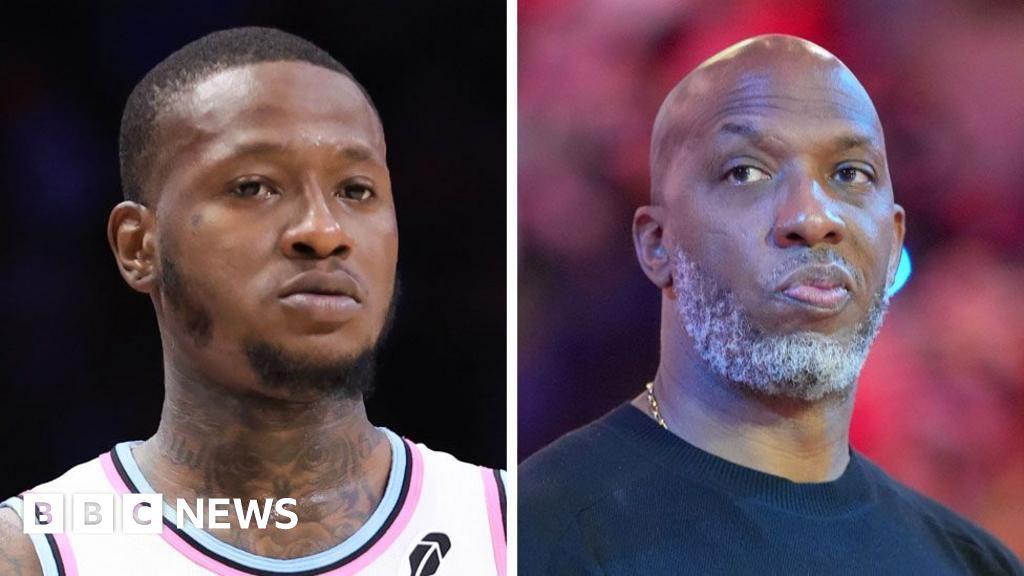
 Marie Fuller
Marie FullerBut even when people can access all the available help, it is sometimes not enough.
Graham and Marie Fuller, from Norwich, contacted the BBC to say their daughter had been hospitalised with OCD aged 12.
They described a revolving-door pattern of going backwards and forwards between NHS services for different treatments, with their daughter improving and then repeatedly relapsing.
After years of their daughter struggling with the condition, the family then decided to go to Texas to try a rare and radical procedure.
Their daughter, who is now 20, underwent deep brain stimulation (DBS) surgery – where electrodes are implanted in the brain to deliver electrical impulses to help manage OCD symptoms.
The treatment is approved by US regulators, but in the UK the National Institute for Health and Care Excellence (NICE) says DBS can only be used for research studies, because there is not enough evidence on how safe or effective the practice is for OCD.
Having a loved one with OCD “has taken its toll on all of us, but we had to do all we could to help”, says Marie, explaining how, before undergoing DBS, her daughter had discussed going to Switzerland to end her life.
Marie says her daughter is now back at university, though she concedes it is still early days in terms of the success of the treatment.
The UK’s health guidelines for obsessive compulsive disorder are 20 years old – they are currently being reviewed by NICE. In 2019, it was agreed that policy around OCD treatment needed to reflect updated technologies and possible new drugs.
But for Leigh Wallbank from OCD Action she says better funding is imperative if young people are to get the help they need.
“Policymakers and the government need to invest in OCD services. [OCD] is preventable and it is a crisis that can be changed.”
A spokesperson for the Department of Health and Social Care said the government had inherited a broken NHS with mental health services suffering following years of neglect – adding that funding was now being boosted by £688m.
But people with OCD such as Sophie are scared about what the future holds.
The limited course of CBT that she’s been prescribed is coming to an end and she fears a return of her symptoms.
“What am I going to do? What if it happens again?”













Leave a Reply