Cancer immunotherapy has long promised a future where the body’s own immune system could become its greatest weapon. That future may now be within reach, as scientists have developed an “off-the-shelf” cancer vaccine that trains the body to recognize and attack tumors carrying one of the most common cancer-driving mutations, known as KRAS. Early results from researchers at UCLA Health and partnering institutions have revealed that this vaccine, called ELI-002 2P, is producing robust and lasting immune responses in patients with pancreatic and colorectal cancer. These two cancers are often considered among the most challenging to treat, with high recurrence rates and limited options once standard therapies have been exhausted.
What sets this approach apart is its simplicity and accessibility. While many cancer vaccines must be custom-made for each individual, a process that can take months and cost a fortune, ELI-002 2P is standardized. It is designed to target a mutation that drives tumor growth in large numbers of patients, meaning it can be administered without the lengthy, personalized preparation typical of most cancer immunotherapies. This could mark a major step toward making advanced cancer treatments more widely available. In early trials, the vaccine not only prompted the immune system to generate cancer-fighting T cells in the majority of participants but also appeared to reduce the likelihood of recurrence, suggesting it might offer a valuable safeguard for patients who have already undergone surgery.

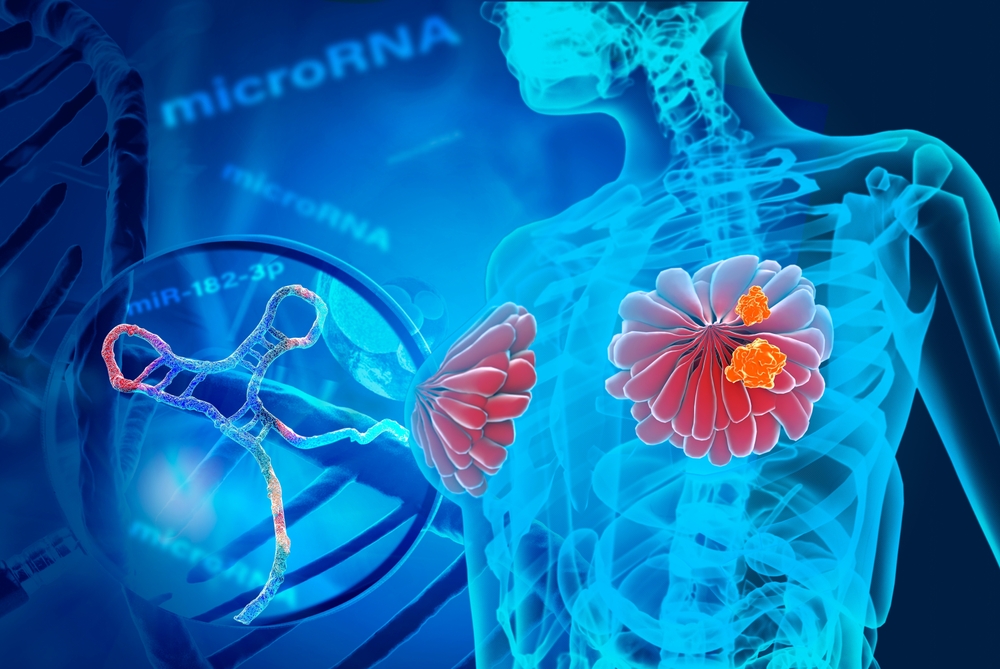
How This Off-the-Shelf Vaccine Works
The science behind ELI-002 2P is elegant in its simplicity. It targets mutations in the KRAS gene, a notorious driver of tumor growth that is responsible for nearly 90 percent of pancreatic cancers and about half of colorectal cancers. Instead of trying to block the mutation directly with drugs, which has proven extremely difficult for decades, the vaccine trains the immune system to recognize and attack any cells carrying it. To do this, researchers employed a specialized amphiphile technology that allows vaccine antigens to travel directly to the lymph nodes, the command centers of the immune system where white blood cells learn to identify threats. Once there, these antigens stimulate both CD4+ helper T cells and CD8+ killer T cells, which together orchestrate a coordinated immune response against the cancer cells.
This approach effectively converts the patient’s own immune system into a surveillance network. Even after treatment, immune memory cells remain vigilant, ready to recognize and destroy any returning cancer cells before they can form new tumors. In this way, ELI-002 2P functions both as therapy and as prevention, potentially reducing the odds of relapse after surgery. Because it does not rely on each patient’s unique tumor DNA, the vaccine can be mass-produced and distributed far more efficiently than personalized alternatives. If ongoing studies confirm these early results, this strategy could open the door to a new era of scalable, precision immunotherapy that combines scientific sophistication with real-world accessibility.
Why KRAS Mutations Have Been So Hard to Target
The KRAS gene has long been considered one of oncology’s most stubborn adversaries. Mutations in KRAS essentially lock the gene in a permanently “on” position, forcing cells to grow and divide uncontrollably. For years, scientists attempted to design drugs to block this activity, but the gene’s structure made it difficult to target without disrupting normal cell function. In cancers such as pancreatic ductal adenocarcinoma, KRAS mutations drive nearly every case, contributing to the disease’s aggressiveness and resistance to treatment. Even when tumors are surgically removed, relapse is common because microscopic cancer cells carrying KRAS mutations often remain behind, ready to reignite tumor growth.
Colorectal cancers driven by KRAS mutations face similar challenges. These mutations render many targeted drugs ineffective, leaving chemotherapy and radiation as the main treatment options. For patients who relapse, choices are limited, and prognosis tends to be poor. By redirecting the immune system’s focus to these mutated cells, ELI-002 2P circumvents the chemical complexity of drug-based solutions altogether. It doesn’t try to inhibit KRAS at the molecular level but instead empowers the immune system to recognize it as an abnormal signature and destroy any cells bearing it. This shift from chemical intervention to immune activation represents a subtle but profound change in how scientists think about cancer therapy, moving from treating the tumor to retraining the body’s natural defenses.

What the Clinical Study Found
The early results from the AMPLIFY-201 Phase 1 trial, published in Nature Medicine, offer cautious optimism. The study followed twenty-five patients, including twenty with pancreatic ductal adenocarcinoma and five with colorectal cancer, all of whom had undergone surgery to remove their primary tumors. Each participant showed signs of minimal residual disease, meaning that traces of tumor DNA were still detectable in their blood. This condition often precedes relapse, making it a particularly vulnerable stage for patients. The vaccine was administered through a series of injections, each designed to reinforce and sustain the immune response over time.
After nearly twenty months of follow-up, the results were striking. Eighty-four percent of patients generated KRAS-specific T cells, and those who mounted stronger responses experienced dramatically better outcomes. Their median relapse-free survival time had not yet been reached, meaning that most remained cancer-free for the duration of the study, compared to a median of just over three months for those with weaker immune responses. Overall survival followed a similar trend, with patients showing higher T-cell activity living well beyond typical survival averages for these cancers. In six patients, including both pancreatic and colorectal cases, tumor biomarkers completely disappeared from the blood, suggesting that the vaccine’s immune response may have cleared residual disease entirely. Furthermore, two-thirds of the participants also developed immune responses to other tumor-associated mutations, indicating that the vaccine’s benefits may extend beyond KRAS alone, potentially training the immune system to recognize a broader range of cancer signatures.
Why This Matters for the Future of Cancer Care
If these findings hold up in larger and longer trials, the implications for cancer care are immense. For decades, the idea of a universal cancer vaccine has existed mostly in theory. Personalized cancer vaccines, though scientifically promising, have remained inaccessible to most patients due to cost, time, and manufacturing challenges. ELI-002 2P challenges that limitation by offering a scalable approach that retains much of the specificity of personalized immunotherapy without its logistical barriers. Its next-generation version, ELI-002 7P, currently in Phase 2 testing, is designed to target an even wider set of KRAS mutations, potentially broadening its reach across multiple cancer types.
This kind of technology represents a bridge between advanced biotechnology and public health practicality. In an ideal scenario, such vaccines could one day be integrated into standard post-surgery treatment for high-risk cancers, much like flu or HPV vaccines are used preventively. Instead of merely responding to relapse, medicine could finally begin to proactively fortify the immune system against recurrence. This also underscores the growing understanding that cancer is not only a disease of rogue cells but also of immune evasion. Restoring immune vigilance might prove as important as targeting tumors directly.

Supporting Immune Health Naturally
While clinical innovation drives medicine forward, supporting immune resilience through everyday lifestyle practices remains foundational. Your immune system responds to the overall balance within your body, and nurturing it naturally can complement modern medical therapies. A diet rich in antioxidants, phytochemicals, and healthy fats supports immune signaling and reduces chronic inflammation, which can weaken immune vigilance over time. Foods such as turmeric, garlic, green tea, citrus fruits, berries, and leafy greens contain natural compounds that strengthen immune pathways. Likewise, maintaining stable blood sugar, staying hydrated, and limiting processed foods helps sustain an internal environment where immunity can thrive.
Regular physical activity enhances circulation and lymphatic function, improving the immune system’s ability to detect and respond to threats. Even gentle exercise such as walking or yoga promotes the flow of immune cells throughout the body. Quality sleep is another cornerstone. During deep rest, the body produces cytokines and growth factors essential for cellular repair and immune regulation. Chronic stress, on the other hand, dampens immune function by increasing cortisol levels, making stress reduction an equally important aspect of wellness. Simple practices such as meditation, breathwork, or spending quiet time in nature can help restore physiological balance. These natural measures do not replace medical treatment but strengthen the foundation upon which therapies like vaccines can work more effectively.

A New Era of Immune-Based Healing
The development of ELI-002 2P represents more than an incremental advance in oncology. It symbolizes a growing convergence between cutting-edge science and the body’s intrinsic healing intelligence. For cancers like pancreatic and colorectal, which have long been associated with grim prognoses, this vaccine offers something rare: genuine hope for durable remission. The idea that a patient’s own immune system can be trained to prevent cancer from returning is transformative, not just medically but philosophically. It reframes cancer care as a partnership between modern biotechnology and the body’s natural defenses.
As researchers continue to evaluate this vaccine in larger populations, the evidence so far points toward a future where cancer prevention and control could depend as much on immune education as on chemical treatment. For patients, families, and practitioners alike, it signals a shift in how we think about resilience, recovery, and the potential to live beyond diagnosis. Even as science continues to refine these tools, the lesson remains timeless: a strong, balanced immune system is both our oldest ally and our most promising frontier.




Leave a Reply