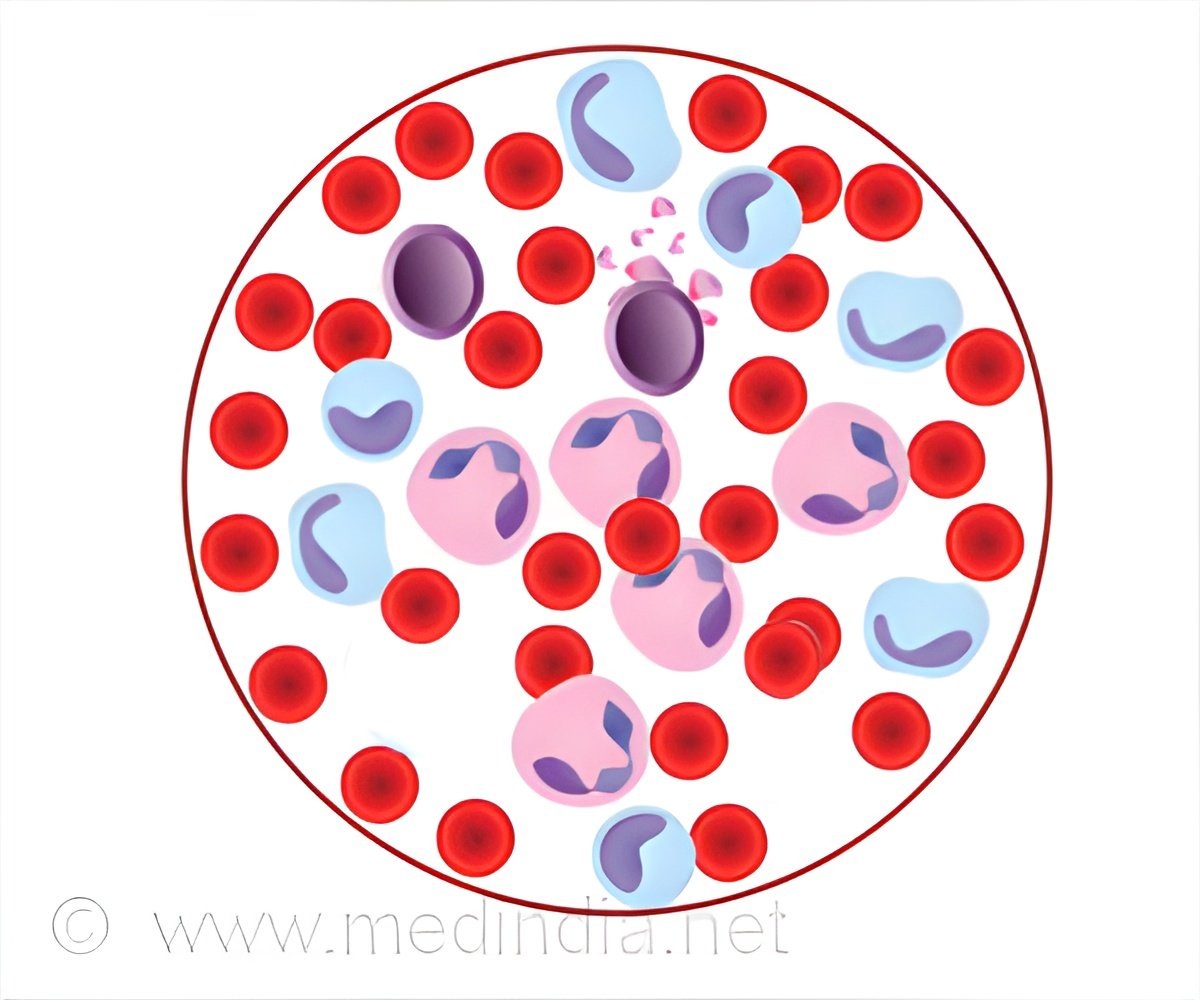
Childhood leukemia is a type of cancer affecting the blood and bone marrow, where abnormal white blood cells grow uncontrollably, affecting the immune system.

Childhood leukemia treatment could become more targeted and less harmful by improving diagnostic accuracy. By examining DNA methylation patterns in leukemic cells, researchers can better assess risk levels—ensuring that only high-risk children undergo the most aggressive treatments. ()
“The healthcare system has become much better at saving lives in childhood leukemia, but the downside of intensive treatments is severe side effects. Our results show that DNA methylation analysis may be a viable way to individualize treatment according to the type of leukemia, with the hope of a better quality of life,” says Professor Sofie Degerman at Umeå University, who has led the study with participating researchers from several countries.
Optimizing T-ALL Treatment: Balancing Efficacy and Long-Term Side Effects
The subtype of leukemia that the researchers in Umeå have studied is T-cell acute lymphoblastic leukemia, T-ALL. The treatment mainly consists of chemotherapy, administered over two years, and in some cases supplemented with a bone marrow transplant. Treatment is usually effective; today, almost nine out of ten children diagnosed with T-ALL survive. The problem is that the treatment causes side effects in the form of nausea, fatigue, susceptibility to infection and hair loss. In the long term, there is also a risk of heart problems, cognitive impairment, fertility problems and suffering from other cancers. The risk of relapse varies within the T-ALL patient group, but it is difficult to determine the risk of relapse with today’s methods of diagnosis. This means that many children receive more demanding treatment for safety’s sake and thus risk more side effects than they might need. One conclusion of the Umeå researchers’ study is that analysis of DNA methylation patterns at diagnosis could contribute to a refined risk stratification to determine which children need which treatment. The method also identifies those patients who respond poorly to current treatments, and these patients may be in need of new treatment strategies.
“The method is already used in several hospitals in the diagnosis of brain cancer, and our study shows that it could also be implemented for leukemia,” says Fernanda S. Hackenhaar, Department of Medical Biosciences at Umeå University, who has contributed to the study’s bioinformatic analysis.
Methylation is an epigenetic process in which chemical groups are added to the DNA sequence, influencing which genes should be expressed and which genes should be silenced. This process occurs in every genome. The methylation pattern varies between different cell types and contributes to cells unique characteristics and properties. If the methylation pattern is disrupted, it can contribute to tumour development. In a way, the DNA methylation pattern acts as a kind of molecular fingerprint, that can provide detailed insights about the properties of the cancer cells. “We are continuing our research to investigate the possibility of including DNA methylation analysis in clinical diagnostics for patients with T-ALL,” says Sofie Degerman.
The current study includes diagnostic leukemia samples from 348 children with T-cell acute lymphoblastic leukemia (T-ALL) treated between 2008 and 2020 in the Nordic countries and in the Netherlands. The researchers have used advanced array technology and bioinformatics to analyse the methylation patterns of approximately 850,000 DNA methylation positions in the genome.
This work will continue in future studies with the aim of further improving treatment strategies.
Reference:
- CpG island methylator phenotype classification improves risk assessment in pediatric T-cell acute lymphoblastic leukemia – (https://ashpublications.org/blood/article/145/19/2161/535228/CpG-island-methylator-phenotype-classification)
Source-Eurekalert












Leave a Reply