Bill and Shelly Gall
The early retirees, who are on an insurance plan purchased through the Affordable Care Act marketplace, spent upwards of $20,000 on health-care expenses and insurance premiums in 2023 and in 2024, largely due to chronic health issues and emergency eye surgeries. The couple is on pace for a slightly smaller sum this year, if they’re lucky, Bill said.
But next year, the Galls, who live in Meridian, Idaho, are bracing for their costs to grow significantly.
Based on figures available through Idaho’s online insurance marketplace, Bill, 61, and Shelly, 60, expect to pay almost $1,700 in monthly health insurance premiums in 2026 if enhanced premium tax credits expire at the end of this year as scheduled. That sum — a nearly 300% increase from their current $442 premium — would add $15,000 a year to their household medical costs.
CNBC reviewed the Gall family’s household financial records, including tax returns and health and insurance documents.
The Galls are among roughly 22 million ACA marketplace enrollees — about 92% of all enrollees — who face the prospect of higher premiums in 2026, according to KFF, a nonpartisan health policy research group.
Democrats are pushing Republicans to extend the enhanced subsidies that make enrollees’ health premiums cheaper, as part of a deal to end the federal government shutdown that began Oct. 1. Republicans have said they want to negotiate any extension of ACA subsidies outside of legislation that would reopen the government.
‘Most vulnerable’ to cost hikes
Early retirees such as the Galls face a bigger financial hit than most if Congress doesn’t act.
The average ACA marketplace enrollee faces a 114% increase in premium payments without the enhanced subsidies, according to KFF.
But older middle- to high-income adults who are too young to qualify for Medicare face the largest dollar increases in premium payments, according to analyses by KFF.
They are perhaps “the most vulnerable population” when it comes to expiring subsidies, said Lynne Cotter, senior health policy research manager at KFF.

Such ACA enrollees who opt to keep their insurance plans might pay 30% of their total annual household income toward health premiums alone, Cotter said.
For comparison, the average household with employer-sponsored coverage spent about 2% of its annual income on premiums in 2024, according to an analysis by KFF and the Peterson Center on Healthcare. That same year, ACA premiums were capped at 8.5% of a household’s income.
“People like us, we need insurance,” said Bill, a civil engineer who retired in 2022.
If the Gall family’s health insurance premiums jump and their medical expenses remain steady, the tally would likely represent more than a quarter of their annual income.
With significantly higher health premiums, the couple said, they would have to make tough financial and lifestyle decisions: pulling more money from retirement savings; claiming Social Security earlier than planned, which would lock in a lower lifetime benefit; putting off non-mandatory medical care; and traveling less.
“If there are no subsidies, we’ll pay the difference. We’ll be out there paying the $1,700 a month,” Bill said. “You do the math. It’s a lot.”
How ACA enhanced premiums work
Subsidies — also known as premium tax credits — have been available since the early days of the Affordable Care Act.
They were originally available for households with incomes between 100% and 400% of the federal poverty level. For a family of two, that equates to an annual income of $21,150 to $84,600 in 2025, according to federal guidelines.
Initially, ACA enrollees whose income went even one dollar over the 400% income threshold weren’t eligible for premium tax credits — a point known as the “subsidy cliff.” In this case, they’d pay the full unsubsidized cost of insurance premiums on the marketplace.
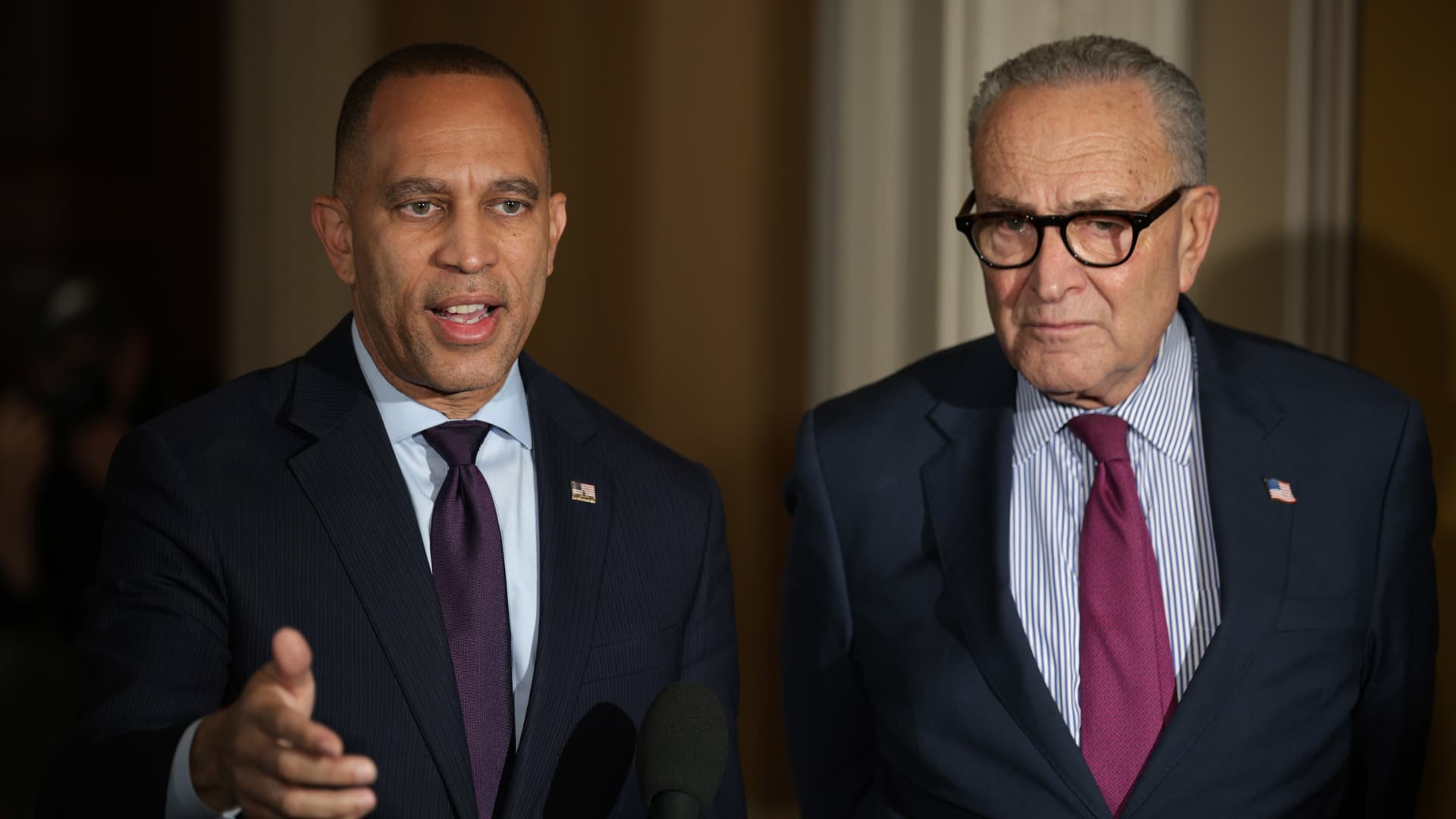
U.S. House Minority Leader Hakeem Jeffries (D-NY) speaks during a press conference at the U.S. Capitol on the third day of a partial government shutdown, on Capitol Hill in Washington, D.C., U.S., October 3, 2025.
Nathan Howard | Reuters
In 2021, the American Rescue Plan Act, a pandemic relief law, raised the value of the premium tax credits and expanded the group of households eligible for them.
These “enhanced” subsidies became available to households with incomes exceeding 400% of the federal poverty line. A household’s financial obligation for premiums was also capped at 8.5% of its income.
In 2022, the Inflation Reduction Act extended the enhanced subsidies and made them available through 2025.
The enhanced tax credits meant families like the Galls qualified.
The couple had a modified adjusted gross income of about $123,000 in 2023 and $136,000 in 2024, mostly from pensions and some from individual retirement account withdrawals, according to their tax returns. Modified adjusted gross income is an income measure used to calculate eligibility for premium tax credits.
U.S. House Speaker Mike Johnson (R-LA) holds a press conference weeks into the continuing U.S. government shutdown in Washington, D.C., U.S., Oct. 15, 2025.
Elizabeth Frantz | Reuters
Enrollment in the ACA marketplace more than doubled since the introduction of the enhanced credits, to 24 million people from about 12 million, according to KFF.
While the percentage of Americans who have ACA marketplace health insurance is small, the share could be large enough to swing a close election, KFF reported in October.
Most ACA marketplace enrollees — 57% — live in congressional districts represented by Republicans, according to the KFF report. At least 10% of residents in all of the congressional districts in Florida, Georgia, Mississippi and South Carolina, and almost all of the districts in Texas and Utah, have Marketplace plans, according to KFF.
The KFF report said that in the 10 most competitive districts in the last election, the margin of victory was fewer than 6,000 votes and that there are at least 27,000 enrollees in each of these districts.
Why early retirees face higher premiums
Extending the enhanced subsidies would cost $350 billion over 10 years, according to the Congressional Budget Office. That’s an average of about $35 billion a year.
If Congress opts to let the enhanced subsidies lapse, many households would still be eligible for premium tax credits, though they’d receive less assistance.
The subsidy cliff would also return, meaning families like the Galls wouldn’t qualify for any premium tax credits.
Without enhanced subsidies, the average 60-year-old couple making $85,000 a year — 402% of the federal poverty line — would see their premiums increase by about $1,900 per month, according to a KFF analysis. Their annual premiums would rise by nearly $23,000 in 2026, KFF found.
About 51% of ACA market enrollees with incomes exceeding the threshold of four times the poverty level are ages 50-64, according to KFF.
Bill, who worked for more than 31 years in local and state government in Nevada and Idaho, said he expects their household to get pension income of about $127,000 in 2026, exceeding the 400% threshold.
The KFF analysis also accounts for the general growth in health-care premiums from year to year; KFF expects a median increase of 18%.
Insurers can generally raise costs more for older adults than younger ones due to the practice of age rating, KFF’s Cotter said. Older people tend to have more health conditions and use their insurance more often; insurers in all states except New York are allowed to charge them higher premiums, she said.
Coping with higher premiums
Bill Gall has what he calls “old eyes”: He’s had more than 10 eye surgeries over the past decade and is now blind in one eye, he said.
Shelly has had two spinal fusion surgeries and suffers from chronic pain, which has prevented her from working full-time since 2015, the couple said. Before that, she had various roles at banks and then in state employment, interspersed by time outside the workforce raising their three sons.

Bill decided to retire early so the couple could enjoy nonworking years together while they’re still in relatively good health, they said.
The couple said they’re limited in their choice of health plan on the ACA marketplace. For example, their various doctors don’t accept certain plans that might be cheaper, they said.
They are enrolled in a high-deductible health plan, with a $12,500 annual deductible and a $15,000 out-of-pocket maximum. They generally budget for that maximum, and reached that ceiling in 2024.
If they lose the enhanced subsidies and their financial load becomes too challenging, Bill could try to find part-time work, he said.
“I don’t want to,” he said. “I have one eye, and it doesn’t work very great.”
Ultimately, Bill said he expects Congress to extend the enhanced subsidies at the last minute.
But he said he worries about the damage it could cause if lawmakers wait too long. People in most states can start signing up for 2026 health-care coverage through the ACA marketplace on Nov. 1.
People may choose not to sign up if lawmakers were to pass an extension far beyond this date, according to analysts.
The Center on Budget and Policy Priorities, a nonpartisan research and policy institute, said in a Sept. 22 report that if the tax credit enhancements are extended before ACA open enrollment begins, people who visit the ACA Marketplace site to shop for coverage will see accurate premium estimates for 2026. If they see the higher premiums that will kick in if the credits are not extended, many will decide coverage is financially out of reach, and getting them to return to the site will be difficult, the report said.
But the Galls are cautiously hopeful.
“I think we’ll get the subsidy,” Bill said. If that doesn’t happen, “it would be a significant cost to us,” he said.













Leave a Reply